Your Guide to Does Mri Show Arthritis
What You Get:
Free Guide
Free, helpful information about Arthritis FAQ and related Does Mri Show Arthritis topics.
Helpful Information
Get clear and easy-to-understand details about Does Mri Show Arthritis topics and resources.
Personalized Offers
Answer a few optional questions to receive offers or information related to Arthritis FAQ. The survey is optional and not required to access your free guide.
Can MRI Detect Arthritis?
Imagine waking up one morning and feeling stiffness in your joints that's more than just the lingering effects of sleep. Is this a sign of arthritis? For many, understanding the nuances of this condition is challenging, and often, the discussion begins with imaging—especially the role of MRI in detecting arthritis. Let's delve into how this advanced imaging technique contributes to understanding arthritis, its effectiveness, and the broader implications of its findings.
Understanding Arthritis: The Basics
Arthritis is an umbrella term used to describe over 100 types of joint diseases. Each type involves different symptoms, with the commonality being joint pain and inflammation. Conditions like osteoarthritis and rheumatoid arthritis are among the most prevalent.
How Arthritis Impacts the Body
- Osteoarthritis (OA): Often described as "wear and tear" arthritis, OA is mainly about the degradation of cartilage in the joints.
- Rheumatoid Arthritis (RA): This form is an autoimmune disease where the body's immune system attacks the synovium, resulting in inflammation and joint damage.
Understanding the specific type of arthritis a patient is dealing with is crucial for tailored management and treatment strategies.
Why Imaging?
Before diving into the MRI specifics, it's essential to understand the role of imaging in diagnosing arthritis. Physicians use imaging to visually assess the structural condition of bones and joints. This aids in:
- Confirming the diagnosis of arthritis.
- Determining the severity of the condition.
- Tracking the progression of the disease over time.
MRI's Role in Arthritis Detection
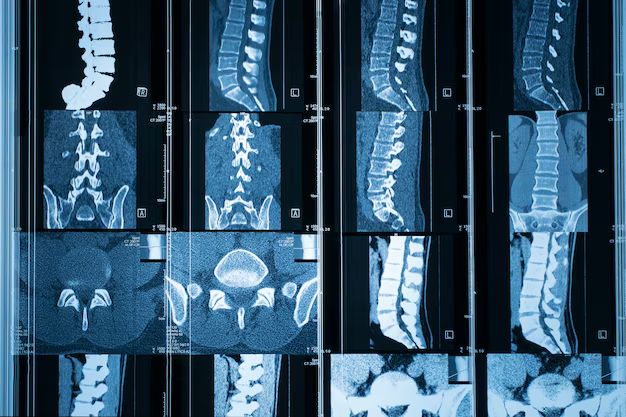
Magnetic Resonance Imaging (MRI) is a non-invasive diagnostic tool that provides detailed images of bones, joints, and soft tissues. Unlike X-rays, which are typically used to view bone, MRI excels in showing soft tissue conditions, making it invaluable for arthritis diagnosis.
How MRIs Work
An MRI uses powerful magnets and radio waves to create detailed images of the inside of your body. These images can then be used to evaluate:
- Cartilage: Helps in assessing deterioration or damage.
- Synovium: Can show inflammation, a common feature in RA.
- Bone Marrow: Changes might indicate infection or inflammation.
- Soft Tissues: Identifying tears or damages to surrounding ligaments and muscles.
What MRI Can Reveal About Arthritis
- Early Detection: MRI can detect early changes in cartilage and other soft tissues long before other imaging techniques.
- Disease Activity: It helps gauge the current inflammatory activity, especially in autoimmune-related arthritis.
- Assessment of Treatment Efficacy: Monitoring changes in MRI images over time can help assess how effective a treatment is.
Limitations of MRI in Arthritis Diagnosis
While MRIs are incredibly revealing, they are not without limitations:
- Cost and Availability: MRI can be more expensive and less accessible than other imaging forms.
- Duration and Discomfort: Some patients find the process lengthy and uncomfortable due to the noise and enclosed space.
- False Positives/Negatives: Occasionally, an MRI can show abnormalities that do not cause any arthritis symptoms, or it might miss subtle changes.
When is an MRI Recommended for Arthritis?
Not every arthritis patient requires an MRI. Physicians typically reserve MRI for ambiguous cases or when conventional methods fail to provide clarity. Here are some scenarios where an MRI might be particularly helpful:
- Persistent, unexplained joint pain.
- To differentiate between types of arthritis.
- When planning complex treatments or surgeries.
- Monitoring disease progression or treatment efficacy.
Other Imaging Techniques: A Comparative Insight
While MRI is a robust tool, it's often used in conjunction with other imaging methods. Here's how MRI compares:
X-Rays
- Strengths: Ideal for detecting bone damage and changes in joint alignment.
- Limitations: Poor in assessing soft tissues.
Ultrasound
- Strengths: Excellent for visualizing soft tissues and guiding joint injections.
- Limitations: Highly operator-dependent and less effective in showing deeper structures.
CT Scans
- Strengths: Provides detailed images of the bone.
- Limitations: Involves radiation and less effective for soft tissue imaging compared to MRI.
Each imaging type has its place in the diagnostic toolkit, and often, a combination is used to get a complete picture.
Practical Tips for Patients Considering MRI
For those scheduled or considering an MRI, these tips might be helpful:
- Share Your Medical History: Inform your doctor of any metal implants or pacemakers.
- Comfort Measures: Utilize earplugs or headphones during the procedure.
- Stay Still: Motion can blur images, so keeping still is crucial for accuracy.
Advancing Arthritis Diagnosis: The Future of Imaging
The field of medical imaging is continually evolving. Innovations such as 3D MRI provide even greater detail. Moreover, research is ongoing into portable MRI machines that could bring this advanced imaging right to patients' bedside.
In the quest for personalized medicine, combining imaging findings with genetic data could further tailor arthritis management strategies, offering hope for more precise interventions in the future.
Key Takeaways 🎯
- MRIs excel at detecting early changes in cartilage and soft tissues, crucial for early arthritis detection.
- Cost and accessibility can be barriers, but when necessary, MRI provides invaluable insight not available with other techniques.
- Different imaging techniques complement each other, with each having unique strengths and limitations.
- Future advances promise even more precise imaging, potentially enhancing diagnosis and treatment personalization.
Arthritis is a complex, multifaceted condition, and utilizing every available tool, including innovative imaging techniques like MRI, allows for better management and improved patient outcomes. For those on the journeys of arthritis diagnosis and management, MRI serves as a window, providing a clearer view—a glimpse into the future of personalized healthcare.
What You Get:
Free Arthritis FAQ Guide
Free, helpful information about Does Mri Show Arthritis and related resources.

Helpful Information
Get clear, easy-to-understand details about Does Mri Show Arthritis topics.

Optional Personalized Offers
Answer a few optional questions to see offers or information related to Arthritis FAQ. Participation is not required to get your free guide.

Discover More
- a Septic Arthritis
- Are Bananas Bad For Arthritis
- Are Tomatoes Bad For Arthritis
- Can An Inflamed Nerve Cause Arthritis
- Can An Inflamed Nerve Cause Arthritis In Dogs
- Can An x Ray Show Arthritis
- Can Arthritis Be Cured
- Can Arthritis Be Reversed
- Can Arthritis Become Septic After Infection From Injection
- Can Arthritis Cause Numbness
